COLUMBUS, Ohio — Groups opposed to mandated vaccinations protest on the grounds of the Ohio Statehouse, inside the House Health Committee meets to discuss HB 248 which would prohibit mandatory vaccinations and vaccination status disclosures, Tuesday, August 24, 2021. Graham Stokes/Freelance Photographer
In a sudden and unmistakable shift, Ohio’s vaccine debate transcended from the abstract to concrete.
An inevitable collision looms.
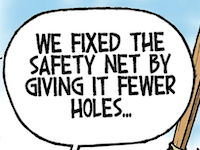
Even before the pandemic, some Ohio Republican lawmakers have sought to limit the ability of businesses — especially hospitals — to require vaccination from employees. This year, lawmakers have held repeated hearings on legislation to ban vaccine mandates from hospitals, nursing homes, colleges and others. The bill covers vaccinations against preventable infectious diseases beyond COVID-19 like polio, measles, flu and more.
The legislation, House Bill 248, would also stop insurers from mandating, incentivizing or even requesting that those within their risk pool get vaccinated.
The legislature is considering this alongside other, narrower proposals. One would only ban state-operated buildings from requiring proof of vaccination to enter. Another would ban COVID-19 vaccine mandates but exempt health care providers, and it would prohibit businesses from incentivizing vaccination or treating unvaccinated and vaccinated people differently.
All this occurs as the hyper-transmissible delta variant of the coronavirus surges in Ohio; hospitals once again sound the alarm about limited care capacities; and Ohio’s adult vaccination rate of 64%, the 13th lowest by state, sags farther behind the national rate of 74%.
Ohio’s institutions aren’t waiting around to see where the Republican-controlled legislature — which has advanced legislation widely opposed by state and federal health officials for nearly the entirety of the pandemic and recently invited testimony from a physician who claimed vaccines “magnetize” their recipients and “interface” with cell towers — lands.
First came the hospitals: Mount Carmel Health announced in early July that all its nearly 12,000 employees must be vaccinated. The Ohio Hospital Association (OHA) recommended its member facilities follow suit; OhioHealth, Ohio State University Wexner Medical Center, Nationwide Children’s Hospital, Kettering Health, Premier Health, MetroHealth, and Dayton Children’s Hospital, just to name a few, did so.
“I think sometimes organizations like hospitals in their communities, they need to take difficult positions and lead,” said Sean McGlone, general counsel for the OHA, in an interview last month.
“I think there is tremendous anxiety in the health care space around the delta variant and the fact that that is a real gamechanger … I think hospital leaders on our board decided we needed to be leaders in this space.”
After the hospitals came the colleges.
Private schools and Cleveland State University started the trend. Then Ohio State University opened the floodgate announcing its vaccine mandate last week, soon followed by Ohio University, Miami University, the University of Cincinnati, University of Akron, John Carroll University and more.
From there, the vaccine mandate list gets a bit more sporadic: the Cuyahoga County Court of Common Pleas; Natalie’s Coal Fired Pizza and Live Music in Worthington; and the Montgomery County Prosecutor’s Office all instituted some kind of mandate. Columbus Alive reports several area concert venues now demand proof of vaccination or negative COVID-19 tests from patrons for entry.
Indeed, the online job posting website, reports a 90% increase over the last month in the number of listings demanding vaccination among new hires.
The state vaccine legislation would pose trouble for insurers as well as those who mandate. In essence, it would force them to assume the potential costs of preventable health care from a COVID-19 hospitalization. It would also forbid them from asking — let alone demanding — their customers take a vaccine that is highly likely to shield them from a hospital trip that costs somewhere between $30,000 and $70,000 a pop.
The state of Ohio has been paying its employees $100 to get vaccinated, and the state Medicaid program is doing the same for its members. Delta Airlines recently announced it would tack a surcharge onto health insurance premiums of unvaccinated employees. HB 248 would outlaw both carrot and stick approaches at the insurers’ expense.
“[Vaccines] are the right thing to do from a public health perspective, but also the right thing to do from a cost perspective,” said Kelly O’Reilly, president and CEO of the Ohio Association of Health Plans.
“When you look at what the cost is for COVID-19 hospitalizations … that’s an absolutely avoidable $30,000 to $50,000 in costs, and ultimately, those costs are costs that are going to be borne by you and I in terms of our health insurance premiums.”
Unsurprisingly, given this dynamic, most of these entities mandating vaccines oppose the GOP legislation. Ohio’s health care providers, the Ohio Chamber of Commerce and health insurers have mounted opposition to the bill. The Inter-University Council of Ohio has registered to lobby on the bill (lobbying records do not specify whether it lobbies for or against).
The bulk of the bill’s support traces to two, active anti-vaccination special interest groups in the state: the Ohio Advocates for Medical Freedom and Health Freedom Ohio. Backers have generally dismissed health concerns related to COVID-19 and reframed the debate around personal liberties and the right to choose — not a duty to protect one’s neighbors.
The vaccine debate is no longer hypothetical in Ohio.
Some of Ohio's most prestigious colleges and hospitals have adopted broad COVID-19 mask and vaccination policies. Will the General Assembly try to stop a moving train?
• • •• • •
This story is provided by Ohio Capital Journal, a part of States Newsroom, a national 501 (c)(3) nonprofit. See the original story here.