The Mercer logo.
When the Ohio Department of Medicaid this year selected six companies to manage $22 billion worth of managed-care business, it was supposed to be a competitive process. But some pretty big questions linger about how competitive it actually was.
Somehow, an Ohio-based company was dinged because it hadn’t worked outside the Buckeye State. But giant, out-of-state bidders got no demerits even though the state in recent years has sued two of them, alleging that they’d defrauded Ohio taxpayers of enormous sums. Some of the litigation isn’t even settled.
But the lawsuits weren’t considered because Mercer, the consulting firm facilitating the process, apparently instructed the Medicaid bigwigs evaluating applications not to. They were told to consider only what was in those applications — not past conduct, Medicaid officials testified in court last week.
It’s unclear whether Mercer and Ohio Medicaid Director Maureen Corcoran might have conflicts of interest. In court earlier this month, a lawyer for the Ohio company that was passed over for the managed-care business asked senior Medicaid officials whether Corcoran filed the same forms they did declaring whether they owned stock in the businesses bidding on the huge contracts. All said they didn’t know. They also said they didn’t know if any of the bidders were among Mercer’s clients.
Corcoran has disclosed that she owned stock in some of the successful bidders since becoming director, but it’s unclear if she continues to do so and she refuses to say whether she filed affidavits disclosing the exact interest she has in them.
Nor will she say whether Mercer, as it was setting up the procurement process, numbered any of the bidders among its clients. Neither will Mercer.
Ambitious plans

When Gov. Mike DeWine, the Ohio General Assembly and the Medicaid department set out to overhaul the program to provide health care to low-income Ohioans, they were trying to tackle some huge problems.
They were working to create OhioRISE, a continuum of services for 60,000 Ohio kids with complex behavioral health needs. The state’s current system is so fragmented that parents of children with the severest problems sometimes have to surrender custody to the state to get their kids all the services they need.
The government officials also were trying to bring transparency to prescription-drug transactions. Using complex, non-transparent methods, prescription middlemen working for Medicaid managed-care providers have up-charged Ohioans by hundreds of millions of dollars a year without touching a single pill.
And, with Ohio’s Medicaid program ranking dismally in terms of health value, officials wanted to refocus the program around the needs of the individuals it serves in an effort to improve outcomes.
To solve the puzzle, the Medicaid department inked three, interrelated sets of contracts.

“What is really the revolutionary component here is that we have looked at all of the most cutting-edge practices, and we are pushing our system to the next generation,” Corcoran said in early April as she announced the contracts, according to The Columbus Dispatch. “The entire country is watching us because there are some really important things we are doing differently.”
The department hired Aetna Better Health of Ohio for $1 billion to stand up OhioRISE and to work with other Medicaid providers to serve the children in the program.
It also hired Gainwell Technologies to be the sole pharmacy middleman. Because it will contract directly with the state, Medicaid officials should have much greater visibility into its activities to ensure taxpayers aren’t ripped off.
And it contracted with six firms to be managed-care companies, meaning they would sign up clients, create networks of providers such as doctors, help determine what’s covered and see to it the providers are paid.
With the vast majority of Ohio Medicaid recipients participating in managed care, the contracts totaling $22 billion made it the biggest public procurement in state history.
Disappointed bidder
When the Medicaid department on April 9 announced five of the six successful applicants for the managed care business, it added three new out-of-state companies to those currently serving the program.

It said it had paused negotiations with health care giant Centene because Attorney General Dave Yost had accused the company of tens of millions of dollars of fraud less than a month earlier.
But after Centene in June agreed to an $88 million settlement, the Medicaid department restarted the talks.
The Medicaid department passed over one current managed-care company, Toledo-based Paramount Advantage. In doing so, the Medicaid department was left with only one Ohio company: Dayton-based CareSource, which also operates in several other states.
Paramount has sued, claiming that it had gotten top scores in the past and that Medicaid officials are biased against it for pointing out that a flawed Medicaid algorithm in 2018 and 2019 had cost Paramount $100 million and crippled the company.
The Medicaid officials who evaluated proposals last week disputed that the incident biased them against Paramount. In court testimony, Medical Director Mary Applegate said that in its application, Paramount didn’t adequately address the change in direction the department is trying to make.
“We wanted resourcefulness,” Applegate said, describing what she thought the Paramount application lacked. “We wanted patient-centeredness. We wanted a new paradigm of what ‘managed care’ means.”
Only consideration
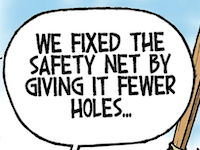
While Paramount and the Ohio Department of Medicaid are disputing the issue of bias, they’re not disputing a crucial factor in the evaluation process: that evaluators had strict instructions not to consider anything other than the applications before them.
That meant they couldn’t consider good scores Paramount got on earlier evaluations. But, perhaps more significantly, it meant evaluators couldn’t consider how some of the country’s largest corporations had been accused of unethical conduct toward Ohio taxpayers — much less taxpayers in other states.
Not only did Centene, the country’s 24th biggest company, pay out $88 million on allegations that it overbilled Ohio taxpayers by tens of millions. It set aside $1 billion more to settle similar claims elsewhere.

Just after announcing the settlement, Centene’s $25-million-a-year CEO in June told investors that his main goal was to make even more money in the future.
The evaluators might have wanted to consider the state’s fraud claims before picking Centene, but they couldn’t if it wasn’t in the company’s application.
The evaluators might also have wanted to consider that in 2019, Yost sued OptumRx, the pharmacy middleman owned by another successful bidder, UnitedHealth Group. Yost claims OptumRx, overcharged the Ohio Bureau of Workers Compensation by $16 million. That case is scheduled for trial next year.
In addition, OptumRx, part of the country’s fifth-largest corporation, was one of two pharmacy middlemen that — according to the Medicaid department’s own investigation — up-charged the department almost a quarter billion dollars in 2017. That set off investigations in Medicaid departments across the country and is largely responsible for the Ohio department’s decision to switch to a single middleman working directly with the state.
The other corporation involved in the massive upcharge is CVS, the nation’s fourth largest company. The Medicaid department awarded its subsidiary, Aetna, the billion-dollar OhioRISE contract.
Not much transparency
The huge upcharges by the middlemen, or pharmacy benefit managers, have been widely ascribed to a lack of transparency in their work. And in announcing the new contracts earlier this year, Corcoran touted the greater transparency the new system would bring to pharmacy benefits.
But Corcoran herself hasn’t been very transparent.
Financial disclosures with the Ohio Ethics Commission indicate that at least from 2019, when she became Medicaid director, through 2020, Corcoran owned stock in UnitedHealth and CVS. For part of 2020, she also owned stock in Humana, another of the six companies that are getting a piece of the $22 billion, five-year, managed care business.
But the Ethics Commission disclosures only require that officials each year list all of the stocks in which they held at least a $1,000 interest during the previous year.
In other words, the filings don’t offer much insight into whether the holdings amount to just a nominal or a serious conflict of interest. If you’ve got just $1,000 worth of stock in a company that gets a mammoth government contract, you might make a little. But if you have $1 million in stocks, you stand to make a lot.
Corcoran won’t say whether she followed a separate law that carries the threat of far more serious civil and criminal penalties, including possibly invalidating the $22 billion worth of contracts Corcoran signed this year. That law says officials such as Corcoran must “prior to the time the public contract is entered into, (file) with the political subdivision or governmental agency or instrumentality involved, an affidavit giving that person’s exact status in connection with the corporation or other organization.”
The Capital Journal asked the Medicaid department how much stock Corcoran holds in companies bidding this year on the huge new business. It also asked informally and through an open-records request for affidavits disclosing those holdings.
“Director Corcoran has followed all applicable laws and the fact that you were even able to write this story, shows that she is complying with disclosure laws,” has so far been the department’s only response.
Corcoran’s department had even less to say about Mercer, the consultant that facilitated a procurement process under which giant corporations’ alleged misdeeds against Ohio taxpayers couldn’t be considered. The department not only refused to answer whether any of the bidders were Mercer clients, it also wouldn’t say how much Mercer was paid for its work.
“Thank you for your questions of Friday and today related to the ongoing litigation in the Franklin County Court of Common Pleas,” spokeswoman Lisa Lawless said Monday in an email. “As you know, that trial continues on November 8, 2021. Ohio Medicaid does not comment on active litigation.”
For its part, Mercer didn’t respond to a request for comment.
Perhaps some answers will be forthcoming when Corcoran takes the stand when the Paramount trial resumes.
• • •• • •