Mint Images/Getty Images.
The Ohio Department of Medicaid plans to radically change the way it does business in July, but a group that helped motivate the reform effort says some fundamental details have not been provided.
Some members of that group, the state’s community pharmacists, say those details could determine whether they can stay in business — and whether some small towns become pharmacy deserts.
The Medicaid department last summer undertook the largest public procurement in state history when it issued $22 billion worth of five-year contracts to six managed-care companies. One goal of the exercise, officials said, was to reorient the program around individual clients and their health.
The state issued another, billion-dollar contract to Aetna to create a continuum of care for 60,000 Ohio children with complex behavior needs. Under the current, disjointed system, some parents have to turn custody of their over to the state to get them the care they need.
And the reforms seek to radically change the way the Medicaid program pays for prescription drugs.
As far back as 2016, independent pharmacists in Ohio and other states have complained that under-reimbursements for Medicaid drugs were driving them out of business. Medicaid managed-care companies hired middlemen known as pharmacy benefit managers to handle the transactions and pharmacists accused the middlemen of starving them while they gouged taxpayers.
The pharmacy benefit managers, or PBMs, say they use their size to negotiate deep discounts from drugmakers, which they say they pass along to consumers.
But the transactions aren’t transparent, and a state audit found that in 2017 PBMs CVS Caremark and OptumRx charged Ohio taxpayers almost a quarter-billion dollars more for Medicaid drugs than they reimbursed the pharmacists who dispensed them. An investigation by The Columbus Dispatch also found that CVS was sending independent pharmacies letters acknowledging that reimbursements were down and offering to buy them out.
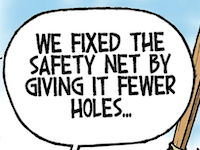
After several attempts at legislative fixes, the Medicaid department is now trying to increase transparency by making the drug middleman — the PBM — work directly for it. Instead of being able to hide behind a contract with a managed-care organization, the new arrangement will give the state total visibility into discounts collected, fees charged and reimbursements made by the new, single PBM.
Instead of being based on some non-transparent, ever-changing reimbursement schedule, the Medicaid department is now trying to come up with a publicly available list of prices it will pay for medicine, plus a dispensing fee to cover pharmacists’ costs.
Problem is, some pharmacies say, the state still hasn’t said what price list it will use or what dispensing fee it will pay.
“We know that what we’ve been paid over the last five years is unsustainable, based on all the pharmacies that have had to close,” said Lynne Fruth, president of Fruth Pharmacy, a chain that operates small-town pharmacies in Ohio, Kentucky and West Virginia.
Fruth shuttered its Nelsonville pharmacy operation in 2019, saying that 50% of its clientele were Medicaid patients and paltry reimbursements from the program made it impossible to stay in business.
Now Fruth is frustrated that she can’t get information from the Medicaid department that will help her allow the company’s 10 other Ohio pharmacies to keep operating.
“The biggest thing is not being able to get anybody to tell us what (reimbursements) are going to be,” Fruth said.
The Medicaid department has said that more transparency is the point of the pharmacy reforms and Director Maureen Corcoran peppers her public statements with that word. However, the department frequently ignores press requests for comment, including for this story.
• • •• • •
This story is provided by Ohio Capital Journal, a part of States Newsroom, a national 501 (c)(3) nonprofit. See the original story here.