Pricing reforms under a sweeping law signed on Tuesday by President Joe Biden are great for diabetics, but much more needs to be done, an activist said Wednesday.
As part of the Inflation Reduction Act, monthly out-of-pocket insulin costs for Medicare recipients were capped by the law at $35 a month. Together with capping all drug costs for Medicare patients at $2,000 a year, the new law is being lauded as a boon for seniors struggling to balance their drug costs with all their other expenses.
Among medicines, insulin is one that is particularly difficult for those who need it to live without. For diabetics, it helps regulate blood-glucose levels that, if left untreated, can cause blindness, nerve and kidney damage and even death.
But even though it’s been around for a century, insulin prices aren’t as cheap as one might think for a class of drugs that has been researched, manufactured and marketed for so long. In fact, until recently, list prices have been increasing rapidly.
“The list price of insulin per milliliter in the United States increased, on average, 2.9% annually from 1991-2001, 9.5% per year from 2002 and 2012, 20.7% annually between 2012 and 2016, and 1.5% per year from 2016-2018,” the American Action Forum reported in 2020.
And that can lead to some excruciating choices if you can’t afford it. The Commonwealth Fund in 2020 reported that among non-Medicare patients, huge numbers had difficulty affording their insulin between 2014 and 2017; from nearly half of the uninsured living below the poverty line to 3% of people with good insurance and who were making five times the poverty level, or nearly $100,000 for a family of four.

“Bottom line for diabetics, we can’t afford to wait,” said John Kennedy, an advocate with Ohio Insulin 4All, said Wednesday in a press conference hosted by the group Protect Our Care.
Kennedy added, “We’re impatient, but our impatience comes from a really good place. It’s because the more time that passes means more diabetics are going to have to make really difficult choices that nobody should have to make; whether to put food on the table or to take the whole dose of their insulin. As we know, about a quarter of all diabetics have said that they ration their insulin supply because they just can’t afford it.”
For Medicare patients, the Kaiser Family Foundation reports that average monthly out-of-pocket insulin costs increased 39%between 2007 and 2020. Now those monthly costs range from $16 to $116, or $192 to $1,392 a year.
With average out-of-pocket insulin expenses for Medicare patients at $54 a month in 2020, the $35-a-month cap in the Inflation Reduction Act represents a more than a 50% savings, KFF reported last month.
While capping those costs — and directly negotiating Medicare insulin prices with drugmakers — is surely welcome news to seniors with fixed incomes, it won’t do much for many other diabetic Americans.
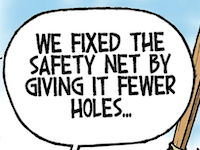
One reason is that the new law keeps intact the opaque system under which giant drug middlemen extract big discounts from drugmakers in exchange for covering them. The three largest middlemen — or pharmacy benefit managers — in the U.S. control more than 70% of the marketplace and each is owned by a corporation that also owns a top-10 insurance company.
And because the system isn’t transparent, it’s unknown how much of the rebates the middlemen and their affiliated insurers are pocketing.
In a paper published last year in the Journal of the American Medical Association’s Health Forum, three researchers at the University of Southern California assed what happened with the prices of 32 insulin products between 2014 and 2018. And despite the fact that drugmakers such as Eli Lilly, Sanofi and Novo Nordisk tend to get most of the blame for rising costs, it shows that others are also culpable:
- List prices went up by 40% while net, or post-rebate, prices received by drugmakers dropped by 31%.
- The share of insulin expenditures retained by pharmacy benefit managers such as CVS Caremark, OptumRx and Express Scripts increased by 154.6%
- The share retained by pharmacies, the largest of which is CVS, increased by 228.8%
- The share retained by wholesalers such as Cardinal Health, AmerisourceBergen and McKesson increased by 74.7%.
While he lauded the insulin measures in the Inflation Reduction Act, Kennedy, the diabetes advocate, they were far from sufficient.
“The way that pricing is done is so hidden; it’s not transparent at all and that’s a big, big, big problem,” he said. “And yes pharmacy benefit managers have played a big role in this secret process — hidden process — that is used to determine what the costs are going to be. But they’re just one player in this game. PBMs certainly share a chunk of the blame, but there’s a lot of blame to go around.”
• • •• • •
This story is provided by Ohio Capital Journal, a part of States Newsroom, a national 501 (c)(3) nonprofit. See the original story here.