Your heart beats around 100,000 times every day. Heart rate is a key marker of cardiovascular activity and an important vital sign. But your pulse is not as steady as a precision clock – nor would you want it to be.
As a cardiovascular physiologist, I measure heart rate in nearly every experiment my students and I perform. Sometimes we use an electrocardiogram, such as you’d see in a medical clinic, which uses sticky electrodes to measure electrical signals between two points of your body. Other times we use a chest strap monitor, like ones you might see on someone at the gym, which also detects heartbeats based on electrical activity.
As wearable technology has grown more popular, it’s not just researchers and cardiologists who are paying attention to heart rate. You might be monitoring your own all day long via a fitness tracker you wear on your wrist. This kind of wearable device uses green light to detect blood flowbeneath your skin and deduces your heart rate.
Here are what heart rate and other measurements derived from this biometric can tell you about your body’s health.
The heart’s primary job is to contract and generate pressure that helps pump blood to the lungs to be oxygenated and then on to the rest of the body to deliver oxygen and other nutrients. Heart rate is simply how fast your heart is beating. Sometimes called a pulse rate, it’s normally presented in beats per minute. You can count your own heart rate by feeling for your pulse inside your wrist or behind your jaw.
When your body demands more oxygen, such as during exercise, heart rate will increase along with the increasing workloads.
While many people are familiar with tracking their heart rate during exertion, the heart rate at rest can also provide valuable information. The two parts of the autonomic nervous system, the sympathetic and parasympathetic, influence resting heart rate. The sympathetic branch helps coordinate your body’s stress response. The more active it is, the higher it dials up your heart rate, preparing you for fight or flight.
The parasympathetic branch of your nervous system is responsible for keeping lots of your body’s functions running smoothly while you’re at ease. Via the vagus nerve that runs from the brain all the way to the abdomen, the parasympathetic nervous system actively slows the heart down to resting values between 60 and 100 beats per minute for the average healthy adult. Without any parasympathetic activity putting the brakes on the sympathetic nervous system’s signals, your heart would beat at approximately 100 beats per minute.
A lower resting heart rate indicates an efficient heart and a higher level of parasympathetic activity. When you’re at rest your nervous system is ideally minimizing sympathetic activity, so you’re conserving energy and avoiding unnecessary stress to the body.
Time between each heartbeat
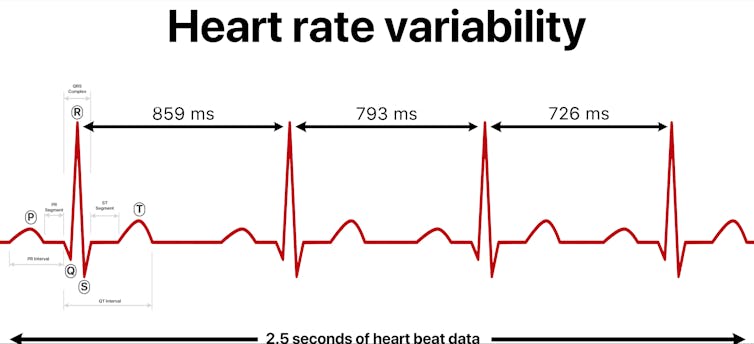
One specific way to understand the balance of the nervous system’s influence on heart rate is to look at heart rate variability, or HRV – the slight fluctuation in the time between each heartbeat. Even if your heart rate is 60 beats a minute, that doesn’t mean your heart is pumping exactly once every second.
Less variability is a sign that your body is under greater stress and that the balance in your autonomic nervous system is tipping toward the sympathetic branch being in charge. Greater variability suggests you’re more relaxed and your parasympathetic nervous system is in control.
For nearly 30 years, scientists have been interested in how to measure and interpret HRV, specifically as it relates to this balance of autonomic control.
The clinical utility of HRV emerged in patients following cardiac events, but researchers are now considering how this measure can help explain patient outcomes in a range of cardiac, endocrineand psychiatric disorders.
More recently, researchers have investigated how to use HRV in athletic training and prognosis of medical conditions.
Several fitness wearables also report heart rate variability, either as a stand-alone metric or used in the calculation of “readiness” or “recovery” scores. Endurance athletes now commonly track HRV as one way to monitor their overall physiological state.
Researchers have started checking which commercially available wearable devices are most reliable and accurate at measuring HRV, which can vary from tracker to tracker. Many of these devices use colored lights, or optical sensors, to measure pulse rate and other variables at the wrist or finger. Unfortunately, the accuracy of this method can vary based on skin type and skin color. It is important that companies include diverse populations in the design, testing and validation of these products to help address potential racial health disparities.

Nudging HRV in a good direction
One of the biggest influences on heart rate variability is stress; along with increased sympathetic nervous system activity, stress is associated with lower HRV. Stress-reducing interventions, biofeedback and increased fitness can increase heart rate variability. Remember, an increase is good for this metric. Overall, heart rate variability depends on a range of physiological, psychological, environmental, lifestyle and nonmodifiable genetic factors.
The most useful way to consider heart rate variability as a metric is to look at data trends. Are there consistent changes in HRV in either direction? Examine these changes alongside other health factors such as fitness, mood, illness, sleep and dietary intake to see if you can draw any conclusions about lifestyle modifications you may want to make.
In general, the same approaches you would take to lowering resting heart rate can also improve heart rate variability, such as increasing cardiovascular fitness, maintaining a healthy weight, reducing stress and getting sufficient sleep.
It’s important to remember that heart rate variability is the normal, healthy, very slight fluctuation of timing of heartbeats – just milliseconds of difference from beat to beat. More dramatic changes in heart rhythms or the way in which the heart contracts, known as arrhythmias, may signal a more serious condition that requires medical attention.
• • •• • •
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Anne R. Crecelius is an Associate Professor of Health and Sport Science at the University of Dayton.