You’ll often hear lawmakers, activists and pundits argue that many transgender people regret their decision to have gender-affirming surgeries – a belief that’s been fueling a wave of legislation that restricts access to gender-affirming health care.
Gender-affirming care can include surgical procedures such as facial reconstruction, chest or “top” surgery, and genital or “bottom” surgery.
But in an article we recently published in JAMA Surgery, we challenge the notion that transgender people often regret gender-affirming surgeries.
Evidence suggests that fewer than 1% of transgender people who undergo gender-affirming surgery report regret. That proportion is even more striking when compared to the fact that 14.4% of the broader population reports regret after similar surgeries.
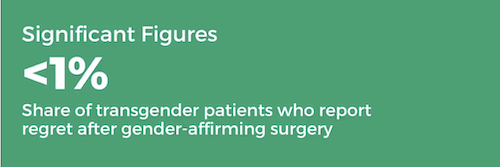
For example, studies have found that between 5% and 14% of all women who receive mastectomies to reduce the risk of developing breast cancer say they regretted doing so. However, fewer than 1% of transgender men who receive the same procedure report regret.
These statistics are based on reviews of existing studies that investigated regret among 7,928 transgender individuals who received gender-affirming surgeries. Although some of this prior research has been criticized for overlooking the fact that regret can sometimes take years to develop, it aligns with the growing body of studies that show positive health outcomes among transgender people who receive gender-affirming care.
Why access to gender-affirming surgery matters
About 1.6 million people in the U.S. identify as transgender. While only about 25% of these individuals have obtained gender-affirming surgeries, these procedures have become more commonplace. From 2016 to 2020, roughly 48,000 trans people in the U.S. received gender-affirming surgeries.
These procedures provide transgender people with the opportunity to align their physical bodies with their gender identity, which could positively impact mental health. Research shows that access to gender-affirming surgeries may reduce levels of depression, anxiety and suicidal ideation among transgender people.
The mental health benefits may explain the low levels of regret. Transgender people have far higher rates of mental health concerns than cisgender people, or people whose gender identity aligns with their sex at birth. This is largely because transgender people have a more difficult time living authentically without experiencing discrimination, harassment and violence.
Gender-affirming surgery often involves going through a number of hoops: waiting periods, hormone therapy and learning about the potential risks and benefits of the procedures. Although most surgeries are reserved for adults, the leading guidelines recommend that patients be at least 15 years old.
This thorough process that trans people go through before receiving surgery may also explain the lower levels of regret.
In addition, many cisgender people get surgeries that, in their ideal world, they wouldn’t receive. But they go through with the surgery in order to prevent a health problem.
For instance, a cisgender woman who receives a mastectomy to avoid breast cancer may ultimately regret the decision if she dislikes her new appearance. Meanwhile, a transgender man who receives the same procedure is more likely to be pleased with a masculine-looking chest.

Improving research and public policy
It’s important to note that this research is not conclusive. Views of surgeries can change over time, and patients can feel quite differently about their outcomes eight years after their surgery as opposed to one year after their surgery.
Nonetheless, the consensus among experts, including at the American Medical Association, is that gender-affirming surgery can improve transgender people’s health and should not be banned.
U.S. states such as Oklahoma and North Dakota have ignored this consensus and have restricted access to these procedures. In response, 12 states have designated themselves “sanctuaries” for gender-affirming care.
Although our statistics on surgical regret may change as researchers learn more, they are the best data that health care providers have. And public policies that are based on the best available evidence have the most potential to improve people’s lives.
• • •• • •