COVID-19 computer generated image. Getty Images.
With nearly 5,000 new cases of COVID per day, Ohio and the rest of the world are still dealing with a pandemic that started nearly two years ago. What we’ve barely begun to deal with, two experts said last week, is the long hangover many experience as “long COVID.”
That expression refers to a set of symptoms that linger for months after a person is infected with coronavirus. They include maladies of the lungs, heart, eyes, liver, brain, bladder, kidneys and pancreas. They also include problems of a less tangible nature, such as a loss of smell, chronic brain fog, headache and fatigue.
And, according to an October study published by the Journal of the American Medical Association, many, many people are likely affected by long COVID. The review of 57 studies found that more than half of the coronavirus patients followed were still suffering from symptoms of long COVID more than six months after they were infected.
With 78% having been hospitalized with COVID, that group appeared to have suffered worse infections than did the general population. Conversely, people who are fully vaccinated are far less likely to be hospitalized, and 49% less likely to develop long COVID, according to a study conducted in the United Kingdom.
Even so, the consequences of the condition are likely to be huge.
Ohio, for example, has seen more than 84,000 COVID hospitalizations, so it seems plausible that well over 40,000 Ohioans have suffered — or are still suffering — long COVID.
Nationally, “you’re talking about 30, 40, 70 million people,” Brett Giroir, who early in the pandemic was assistant secretary of the U.S. Department of Health and Human Services, said last week during a webinar organized by the National Institute for Healthcare Management Foundation.
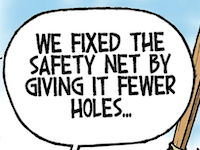
As they were during the early days of the pandemic, policy makers are groping for ways to deal with long COVID without much in the way of scientific information to work with so far.
“We’re unfortunately dealing with from a position of a real lack of knowledge,” Walter Koroshetz, director of the National Institutes of Health’s Institute of Neurological Disorders and Stroke, said during the webinar.
“We’re really trying hard to understand what is the biological basis for the problems that people are experiencing and hoping to get some answers very quickly that can then be used to help patients,” Koroshetz added.
Giroir now is working with the health consulting firm Leavitt Partners on several issues, including problems related to the pandemic. He offered a broad framework for dealing with long covid.
“How do we organize the healthcare sector” in response to long COVID? he asked. “Do we have long COVID clinics. Do we have telehealth triage? How do we care for this 30 to 50% of 140 million people who potentially have long COVID?”
Giroir is proposing several steps to deal with the issue. Among them are helping medically underserved populations through grants to federally qualified health centers and primary-care practices, a national survey on the condition and by working to raise public awareness of it.
• • •• • •
This story is provided by Ohio Capital Journal, a part of States Newsroom, a national 501 (c)(3) nonprofit. See the original story here.